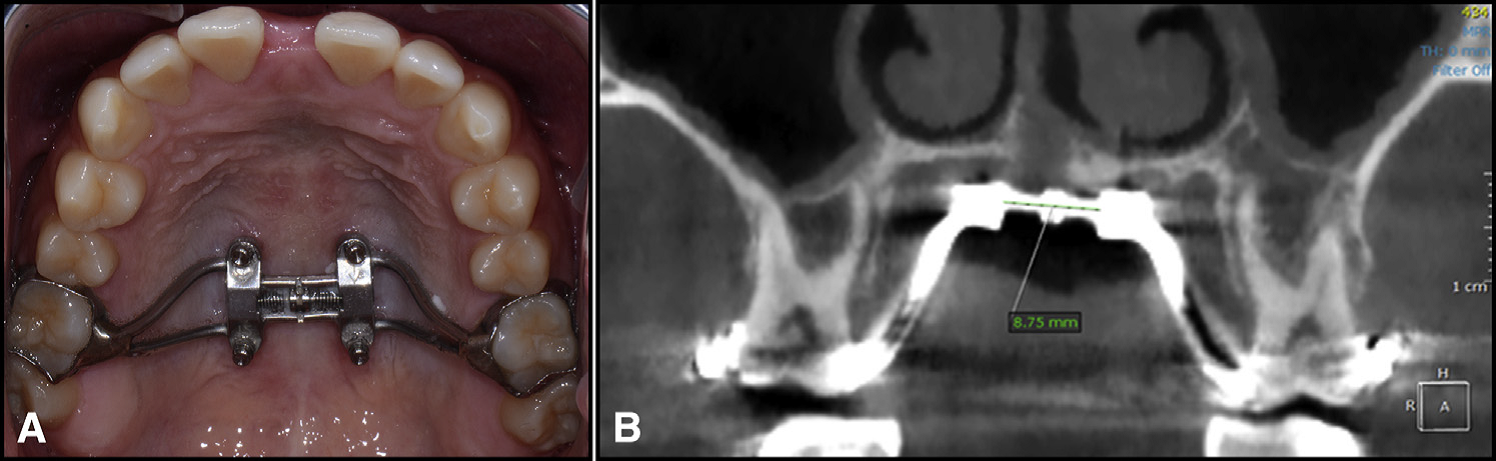
 A modified Wilmes-style expander was used in all patients – with 4 mini-implants in the palate, and attachment to the first molars. (from Cantarella et al.) A modified Wilmes-style expander was used in all patients – with 4 mini-implants in the palate, and attachment to the first molars. (from Cantarella et al.) BY TATE H JACKSON AND TUNG T NGUYEN STUDY SYNOPSIS A group at the University of California at Los Angeles (UCLA) have conducted a retrospective study to evaluate how rapid palatal expansion with mini-implants placed in the palate works in post-pubertal patients. 15 participants (9 female) with ages ranging from 13.9 to 26.2 years were all consecutively-treated with a modified Wilmes-style hybrid tooth-borne / mini-implant borne maxillary expansion appliance. 14 of these patients were in dental crossbite. The need for expansion was determined by measuring and comparing maxillary and mandibular casts, not by comparison to population norms. All participants were treated with the hybrid tooth/mini-implant expander alone; no other appliances were in place during expansion. The authors report that all mini-implants were placed in the posterior palate with bicortical anchorage. The hybrid expander was turned twice each day (0.25mm per turn) until “a diastema appeared” and then just once per day. The expansion devices were maintained for 3 months following the end of activation. Cone-beam CT (CBCT) images were obtained for each participant before treatment and within 3 weeks of the end of active expansion, but before any additional active appliances were placed. After cranial base superimposition of the pre- and post-expansion volumes, transverse expansion was measured in coronal sections at the level of the Upper Zygoma (frontozygomatic suture), Lower Zygoma (zygomaticomaxillary suture), and Maxillary Molars. Expansion resulted in little transverse change at the Upper Zygoma [mean of 0.52mm (SD 0.37mm]. An average of 4.62mm (SD 1.33mm) of expansion occurred at the Lower Zygoma, and 8.33mm (SD 2.29mm) occurred at the Molar. Taken together, for every 1mm of transverse expansion, the zygomaticomaxillary complex rotated outward by 0.6 degrees on each side. Stated another way, an average of 6.8mm in expansion at the level of the jackscrew resulted in an average of 8.33mm of expansion at the molars, with an average of 2 degrees of total outward tipping of the molars on each side. It is important to note that tipping of the molars was highly variable, with standard deviations reported that were nearly double the mean. 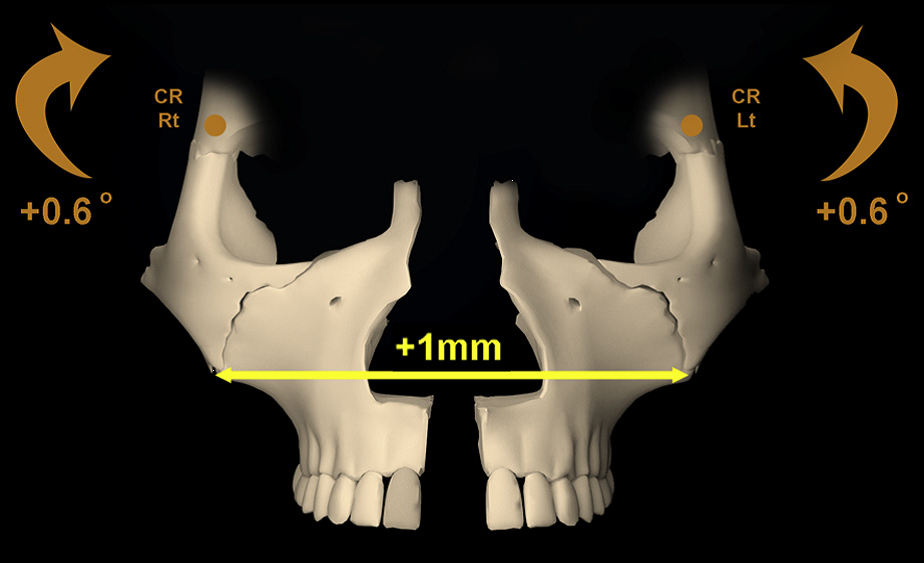 For every 1mm of total expansion at the midline, each half of the zygomaticomaxillary complex rotated outward by 0.6 degrees. (from Cantarella et al.) For every 1mm of total expansion at the midline, each half of the zygomaticomaxillary complex rotated outward by 0.6 degrees. (from Cantarella et al.) WHAT THE PROFESSORS THINK The consecutive case series reported in this paper represents a well-constructed study, despite the limitations of retrospective data analysis. Superimposition of CBCT volumes and analyses of transverse changes were founded on validated methods, and reliability of the measurement made were adequately measured and reported. It is unfortunate that the authors did not report the rate of adverse outcomes for the participants in the study. e.g. Did any of the mini-implants fail? The paper focused a bit more on theoretical biomechanical outcomes, such as where the center of rotation might be for the skeletal units involved, than is likely to be helpful for practicing orthodontists. Some practical points can be gleaned, however: 1. When using a hybrid bone/tooth borne maxillary expander in later-adolescent to early adult patients, you should expect some “tipping” of the molars. That tipping happens due to a combination of skeletal rotation, and to a lesser degree, change in inclination of the molars. 2. Based on this study alone, the amount of molar tipping that occurs can be quite variable. As little as 4 degrees of total tipping might occur, or as much as 10 degrees. From previously published studies, the amount of tipping using mini-implants should certainly be expected to be less than with tooth-borne expansion alone, however. (1, 2) 3. In order to give a patient good estimates of the likelihood of both success and adverse outcomes with this treatment, more data are needed. These data represent good initial guide-points for orthodontists in practice and suggest that mini-implant maxillary expansion should be considered in younger non-growing patients with skeletal transverse issues. The prudent orthodontist, however, will communicate with the patient / parents that although the procedure is a great alternative to more invasive surgery, it still carries with it some real risk and uncertainty at this time. Article Reviewed: Cantarell D, et al. Midfacial changes in the coronal plane induced by microimplant-supported skeletal expander, studied with cone-beam computed tomography images. Am J Orthod Dentofac Orthop 2018; 154:337-345 (Sept). References: 1) Lin L, Ahn HW, Kim SJ, Moon SC, Kim SH, Nelson G. Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015;85:253–262 2) Mosleh MI, Kaddah MA, Abd ElSayed FA, ElSayed HS. Comparison of transverse changes during maxillary expansion with 4-point bone-borne and tooth-borne maxillary expanders. Am J Orthod Dentofacial Orthop. 2015;148:599–607.
1 Comment
john stieber
9/23/2018 12:37:58 pm
I see this is common however nobody wants to take a 6-12 study to evaluate to stability of palatal expansion of any type. My experience (40 yrs) shows that any expansion is transient to a large degree and basing your treatment on this stability is problematic at best. I feel our profession is not willing to face the music in a procedure that has been around for decades yet clinically long tern is highly unstable. If this were not the case, why are we looking at bone borne expansion?
Reply
Leave a Reply. |
Curated by:
Tate H. Jackson, DDS, MS CategoriesArchives
October 2019
|
 RSS Feed
RSS Feed