Clinical Series - Management of Class III Patients Using Bone Anchors: True Orthopedics Part I7/26/2017  BAMP uses only intraoral Class III elastics worn to skeletal anchorage plates to achieve a Tue Orthopedic Effect. BAMP uses only intraoral Class III elastics worn to skeletal anchorage plates to achieve a Tue Orthopedic Effect. BY TUNG T. NGUYEN, DMD, MS & HUGO DE CLERK MS, PHD In 2008, an innovative approach to the treatment of Class III skeletal malocclusions in growing patients was introduced by Hugo De Clerk. Bone Anchored Maxillary Protraction (BAMP) uses intra-oral skeletal plates and intermaxillary elastics (IME) to produce true orthopedic changes by protracting the maxilla and redirecting growth of the mandible, without dentoalveolar side-effect.(1) The purpose of this clinical multi-part series is to summarize 8 years of clinical research on BAMP and give clinicians the tools to apply this protocol to their daily practice. Class III malocclusions are among the most difficult to treat, with a large percentage of these patients requiring orthognathic surgery after mandibular growth is complete (after 16-18 years of age). Ideally, the option of a successful treatment approach that avoids surgery is needed. Such a treatment would:
Conventional treatment for young Class III patients often involves extra-oral devices designed to either increase maxillary length or restrain mandibular growth. Both approaches have had limited success due to undesirable dentoalveolar movements, limited skeletal changes, poor compliance, or relapse of dental movements. Even with appliance modifications to minimize tooth movement and maximize orthopedic correction, some dentoalveolar side-effects are inevitable because these appliances are attached to the teeth. In addition, compliance is critical for success with these treatment modalities. Unfortunately, compliance proves to be difficult, as these cumbersome and socially stigmatizing extra-oral devices require 12-18 hrs of wear per day. Even with good compliance, it is difficult to maintain the correction: 25% to 33% of these patients experience post-treatment relapse within a year.(2) With Bone Anchored Maxillary Protraction, patient compliance was improved due to the discreet nature of intra-oral elastics compared to the cumbersome extra-oral headgear. In addition, our studies showed BAMP was significantly more effective than the current gold standard for early treatment of Class III and can be implemented at a later age.(3) 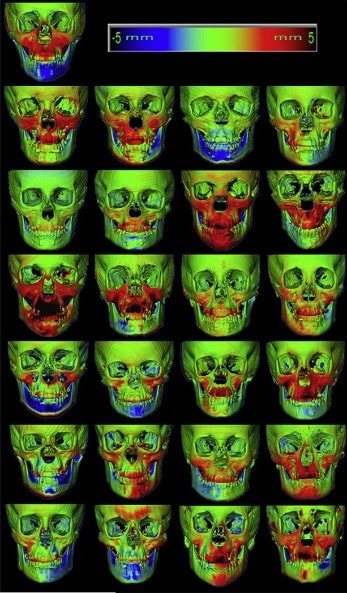 3D Superimpositions showing the orthopedic changes in 25 consecutive BAMP patients. 3D Superimpositions showing the orthopedic changes in 25 consecutive BAMP patients. In this, Part I of our BAMP Series, we will discuss the background and some of the existing evidence for the efficacy of this treatment modality. In later parts, we will discuss the clinical technique, tips, and strategies for managing complications. One of our initial studies involved the 3D analysis of treatment outcomes for BAMP. Twenty-five consecutive Class III patients were enrolled in the study.(4) Using 3D registration of initial and final Cone Beam Computed Tomography (CBCT) for patients treated using the BAMP protocol, we evaluated orthopedic changes in the maxilla, mandible, and glenoid fossa. Using the BAMP protocol, we saw an average anterior displacement in the maxilla by approximately 3.7mm with a range from 1.5mm to as high as 8.5mm. One explanation for the high variations in treatment response between patients might be due to the diversity of the original malocclusions. Some of the Class III patients presented with a severe -5mm overjet while others manifested a mild edge to edge incisor relationship. Other reasons for the high variation in treatment response include compliance with elastics, age, skeletal malocclusion, and maturation of the cranial sutures at the start of treatment. We also saw forward The displacement of zygoma and midface by approximately 3.7mm, a phenomenon that rarely occurs with other treatment modalities. To explain this phenomenon, we examined the circummaxillary sutures and saw that the BAMP protocol resulted distraction of many of these circummaxillary sutures. It may be plausible that a constant force from the elastics, when applied before sutural maturation can effectively produce distraction of these sutures resulting in the forward displace of the entire midface. Recent animal studies have shown that continuous force application is more effective at expanding the sutures when compared to intermittent forces.(5) The changes in the anterior mandibular region were more variable in both magnitude and direction. Many subjects exhibited a distal displacement of the chin, while some continued to grow in a normal forward direction.(6) While the anterior position of the chin stay relatively the same throughout the course of treatment (-0.5mm), this was significant when compared against matched untreated Class III subjects, who showed an mean forward growth of 2.2mm during the same time interval.(1) It is also interesting to note that the BAMP protocol did not restrain growth of the mandible - but instead, it altered the direction of mandibular growth by closing the gonial angle and distalizing the posterior ramus and condyles.(6) The glenoid fossa remodeled to adapt to the new position of the condyle. While these findings are promising; long term studies are needed to evaluate the stability of this compensatory mechanism as well as the health of the temporomandibular joint complex. In summary, BAMP is a promising protocol for true orthopedic treatment, one that has the potential to reduce the need for orthognathic surgery in growing Class III patients. In Part II of our BAMP series, we will address the BAMP clinical technique in detail. References
1 Comment
|
Curated by:
Tate H. Jackson, DDS, MS CategoriesArchives
October 2019
|
Copyright © 2016
 RSS Feed
RSS Feed