 In this study 2mm bite-raisers were bonded on the Maxillary first molars. Photo courtesy of Dr. Phillip Hamilton. In this study 2mm bite-raisers were bonded on the Maxillary first molars. Photo courtesy of Dr. Phillip Hamilton. By TATE H. JACKSON STUDY SYNOPSIS Is it not uncommon to have a patient ask if they will be able to eat and chew with bite raisers (temporary bonding material on the occlusal surface of posterior teeth). A recent study from a group in Thailand has tried to address that question by using both objective and subjective methods. 30 healthy adult dental students (age 18-25, 19 females) without any orthodontic appliances were participants in the study. All had a Class I occlusal relationships with positive overjet, and an overbite of <3mm. None had missing teeth, TM Joint dysfunction, or orthodontic treatment within the previous three years. None had third molars, but all had a full complement of permanent teeth without edentulous areas otherwise. For all participants, chewing ability was measured both objectively and subjectively at two different time points. The objective measure (Masticatory Performance Index, MPI) was calculated as the percentage by weight of standardized food that passed through a standardized sieve after a pre-determined number of chewing strokes. The subjective measure was a validated questionnaire (Food Intake Ability, FIA). At baseline, the objective MPI and subjective FIA were both recorded. Then, one week later, participants had Band-Lok placed on the palatal cusps of the maxillary first molars using a template to create bite-raisers that were 2mm in height. With the bite-raisers in place, chewing ability was again measured using the MPI method and FIA questionnaire. With 2mm bite-raisers in place, the objective ability to chew decreased by an average of 43.3% (P<0.001), while the perceived ability to chew decreased by just 14.6% (P<0.001). Overbite went from an average of 2.35mm before bite-opening to -0.57mm with Band-Lok in place. There were no differences in objective or subjective measures between male and female participants, nor was there any correlation between changes in subjective and objective measures over time across participants. WHAT THE PROFESSOR THINKS
It is the combination of objective and subjective measures of chewing ability using a common clinical technique (Band-Lok on first molars) that gives this study clinical relevance, despite the fact that it was performed under non-clinical conditions. Using dental students with a Class I occlusion controlled for the potential effect of various malocclusions on the ability to chew. The longitudinal design of the study was a strength, as it further helped to control for individual variation in chewing. The use of validated measures was also appropriate. It is key to note, however that these data reflect the ability to chew immediately after bonding bite-raisers. Neither the potential effect of functional adaptation over time nor the effect of changing occlusal relationships during in active treatment were considered. So how then might clinicians use these data in practice? When bonding bite-raisers on molars, orthodontist can use these data to better communicate with patients using the following three points:
THE BOTTOM LINE: We expect patients to adapt to tremendous intraoral changes during orthodontic treatment. When it comes to the ability to chew, these data suggest that even if patients can adapt over time, we should be mindful of the challenges that bite-raisers might pose in the short-term. Article Reviewed: Chidsanu Changsiripuna and Darin Pativetpinyo. Masticatory function after bite-raising with light-cured orthodontic band cement in healthy adults. Angle Orthodontist. Online. 2019.
0 Comments
BY TATE H. JACKSON STUDY SYNOPSIS A new study from a group in Copenhagen addresses a topic that many practicing orthodontists consider on a daily basis: how might intraoral scanning affect patient experience? 59 children (28 female) age 9-15 years were recruited to participate in the study, which took place during 2016 -2017. Of particular note, none of the participants had any prior experience with either intraoral scanning or alginate impressions. Each of the children had an alginate impression made at their first visit, followed by an intra-oral scan (Trios, 3Shape) at the second visit. The same operator, who was a novice in terms of intraoral scanning (calibrated with 10 hours of instruction and 5 practice scans), obtained both the impressions and the scan.  All participants (n=59) experienced an intraoral scan after having experienced an alginate impression. All participants (n=59) experienced an intraoral scan after having experienced an alginate impression. Patients rated comfort in terms of several parameters, including time perception, gag reflex, breathing, and smell and taste. Patients also answered questions that assessed anxiety during each procedure. Additionally, chairside time for each procedure was recorded, a cost estimate for both procedures was made, and dental arch measurements were made to test accuracy. The results:
WHAT THE PROFESSOR THINKS A randomized study design would have been better, because it would have limited the priming or biasing effects that could be created by consistently exposing patients to alginate impressions first. Nonetheless, the longitudinal design in which each patient had both a scan and an impression administered by the same clinician is a strength of the study. Similarly, using a clinician relatively naïve in the use of an intraoral scanner, but presumably more experienced with alginate impressions, lends credibility to the result that scanning truly was more comfortable. The study found that intraoral scanning is just as accurate as using alginate. These results are not surprising. Certainly, the ‘old way’ (alginate) is accurate enough, but now ample evidence confirms that 3D scanning and printing is capable of the accuracy and reliability needed for high-quality patient care. When it comes to patient comfort, these data are more useful:
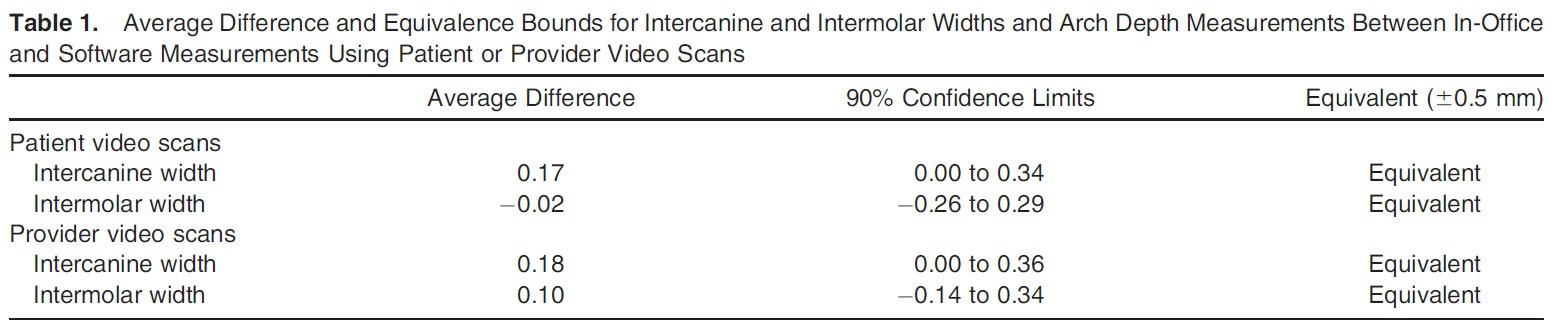
It is not a foreign concept to clinicians in practice that we might purchase costly new technology and then need to ‘justify’ its use in our clinic. To that end, we might be tempted to echo an industry claim that a new procedure or material is faster or more accurate. Now, orthodontists have peer-reviewed evidence that supports the use of intraoral scanners in order to improve the patient experience. Does that mean alginate is no longer ‘standard of care’? Or, that intraoral scanners should be required to meet the standard of care? Certainly not. It does mean that orthodontists can confidently suggest to patients that using an intraoral scanner is an evidence-based effort to provide them with the most comfortable experience possible. Article Reviewed: Olja Glisica, Louise Hoejbjerrea, Liselotte Sonnesenb. A comparison of patient experience, chair-side time, accuracy of dental arch measurements and costs of acquisition of dental models. Angle Orthodontist. Online July 2019. BY TATE H. JACKSON STUDY SYNOPSIS Newly published data from a group at Virginia Commonwealth University examines the accuracy of a smartphone app (in which patients scan their own teeth) in making linear dental measurements during rapid maxillary expansion. 12 patients (age 10-17 years, 4 males) for whom rapid maxillary expansion using a Hyrax appliance was planned were enrolled as a prospective cohort. At baseline, the patients were trained in the use of the app Dental Monitoring (Paris, France). Patients all used the same Apple iPhone 6 Plus and the lip/cheek retractors provided by the company for use with the app while capturing video scans of their own teeth. Before Hyrax delivery, at the time of Hyrax delivery, and then weekly during active expansion, each patient made a scan of their own teeth using the same smartphone at the clinic, in a private room away from the study personnel. For comparison, study personnel also scanned each patient’s teeth using the same app and phone at each visit. Alginate impressions were also made at each visit to serve as a gold standard measure, along with intraoral measurements. Only at baseline was an intraoral scan also obtained using an iTero intraoral scanner. Intermolar and intercanine width measurements were made during the course of expansion using data obtained with the app and compared to measurements made on plaster models. Repeatability of measurements made on the plaster models was high (ICC=0.99). In total, all intermolar and intercanine expansion measures calculated by the app were within 0.5mm of the measures made using plaster casts (Table 1 from Moylan et al). 3 of 58 video scans captured by the app (2 by patient and 1 by study personnel) were judged to be of poor enough quality to not be used for measurements.
WHAT THE PROFESSOR THINKS Although the sample size in the study was small, the fact that multiple video scans were obtained for each participant yielded enough data to draw interesting initial conclusions. The study was well-designed in that the two linear measurements that were evaluated have great clinical significance in the context of rapid maxillary expansion. Similarly, having all patients use the same phone in a private setting away from examiners was logical for the aim of the study, which was to determine the accuracy of patient-obtained intraoral scans using a smartphone. If patients had used a variety of phones in an uncontrolled setting, more confounding variables might have been introduced. This study is well-placed for the current state of orthodontic practice. If a smartphone app can deliver accurate information regarding tooth position that is clinically acceptable (and 0.5mm was a reasonable threshold in this study), certainly clinicians should be open to the judicious use of similar technology for the best care of our patients. In this case, monitoring Hyrax expansion remotely with fewer in-office visits, might be possible. These data do not suggest that “selfie-orthodontics” is appropriate. They do, however, provide good initial data to suggest that orthodontists might have the opportunity to ethically embrace such technology as another tool to provide optimal care. Article reviewed: Heather B. Moylan; Caroline K. Carrico; Steven J. Lindauer; Eser Tu¨ fekci¸. Accuracy of a smartphone-based orthodontic treatment–monitoring application: A pilot study. Angle Orthodontist. Online 2019. First, Do No Harm: Are White Spot Lesions Less Likely to Develop with Aligners? This Study Says Yes.1/27/2019  Initial and final photographs were visually assessed for the presence of white spot lesions. From Buschang et al. Initial and final photographs were visually assessed for the presence of white spot lesions. From Buschang et al. BY TATE H. JACKSON & WILLIAM V. GIERIE STUDY SYNOPSIS: Is oral health better for patients treated with clear aligner therapy? A retrospective study from Texas A&M set out to address that question by comparing the incidence of White Spot Lesions (WSL’s) in two groups of consecutively-treated patients. The aligner group contained 244 patients, while the group treated with braces included 204 patients. 85% of the aligner group were treated in a single private practice, while 52% of the braces group were treated in a single academic setting. There was no statistically significant difference in the gender or age of each group (both had a mean of ~30 years with a standard deviation of 11.5 to 14 years), but there was a difference in treatment duration, with the aligner group treated in less time (1.5 years vs. 2.5 years for braces). At the end of treatment, the aligner group demonstrated a very low incidence of new WSLs, 1.2%, while the group treated with braces had an incidence of 25.7%. For both groups, maxillary teeth were more likely to be affected. Not surprisingly, WSL incidence was lower in the private setting, although the difference in incidence between groups (aligners vs. braces) was consistent in both the academic and private settings. WHAT THE PROFESSORS THINK Although this study suffers from the fact that it is observational and retrospective, there are a couple of key insights to note. Both groups, the aligner group and the braces group, started with a similar pre-treatment prevalence of WSLs : 9% for the aligner group and 10% for the braces group, suggesting that the natural incidence of WSLs in these patients was similar before treatment began. With treatment, only 3 out of 244 aligner patients developed new WSLs, while 52 of 204 patients in braces group did. Given the incredibly low incidence of new WSLs in the aligner group, the authors were wise to only analyze risk factors for developing WSLs in the braces group. As expected, 1) poor oral hygiene that worsened and 2) longer treatment time both increased the risk of WSL development. To most orthodontists in practice these results will be no surprise. Using removable appliances can allow for better oral hygiene – and thus aligners are less likely to be associated with WSL formation. So, does that mean one might use this study to support the use of clear aligner therapy in any patient simply because their hygiene is poor? Certainly not based on that single factor alone. The authors correctly point out that this study does not account for the complexity of the malocclusion or specific treatment mechanics needed. In this study, aligner patients were more likely to improve their oral hygiene during treatment, while braces patients were more likely to worsen. Wearing aligners requires compliance for success – just like oral hygiene. So, are patients who successfully wear aligners more capable of good oral hygiene anyway? This study does not address that question directly, but it does suggest that it might be true. In practice, these data can be used to better communicate with the healthy motivated patient who is concerned about their individual risk for WSLs:
What about the patient who is not motivated? Should aligners be considered for patients who already have WSLs because their risk of new lesions is lower with aligners?
Article Reviewed: Peter H. Buschang; David Chastain; Cameron L. Keylor; Doug Crosby; Katie C. Julien. Incidence of white spot lesions among patients treated with clear aligners and traditional braces. Angle Orthodontist. Online 2018. If You Want Good Oral Hygiene in Your Patients, Text Them Every Day: Data from A Randomized Trial.1/2/2019 BY MATTHEW LARSON & TATE H. JACKSON STUDY SYNOPSIS: 80 patients being treated at the Texas A&M School of Dentistry enrolled in this randomized trial to test whether daily or weekly text message reminders might better improve oral hygiene. At the start of the study, all patients had been in upper and lower fixed appliances for at least 4 weeks, spoke English, were between the ages of 12 and 17 years, and were more than 6 months from the end of active treatment. Patients (not their parents) received texts through a third-party company that provides such services. In that way, the randomized groups could be blinded from the study authors. Patients received one of three types of text messages: 1) oral hygiene texts (e.g. “Don’t forget to brush your teeth twice a day!’’), 2) shorter treatment time texts (e.g. “Your time in braces will be shorter if you keep your mouth very clean!”), and 3) motivational texts (e.g. “Research shows that a better smile leads to better-paying jobs”).  Dr. Matthew Larson Dr. Matthew Larson After 8 weeks of text messages, bleeding, plaque, and gingival indices were all measured by a single blinded examiner. All indices were all significantly lower for the daily text group compared to the weekly text. The largest difference between groups was found in the bleeding index, where number of sites with bleeding on probing decreased 48% in the daily group but only 27% in the weekly group. When surveyed, 97% of patients thought that text messages were helpful, and 70% preferred texts in the evening (7-9PM was the most preferred time). In regards to patient preference on texting frequency, 57% reported they preferred text reminders daily or twice a day, while an additional 20% preferred 3-4 times a week. Texts related to a reduction in treatment time were reported by patients to be most motivational. WHAT THE PROFESSORS THINK This study was well-designed. The use of a third-party company to deliver the text messages was helpful in two ways. First, it allowed for better blinding; the clinicians treating the patients were not responsible for sending the reminder messages. Second, the use of currently-available technology through this service makes the results more likely to be clinically relevant. Although overall well-designed, there are also a few limitations to be discussed. First, it is always difficult observing oral hygiene in studies due to the Hawthorne Effect – oral hygiene will typically improve to some degree simply because patients are enrolled in a study. Also, the daily messaging group had slightly lower periodontal indices at baseline, although only the plaque index was statistically significant. These limitations likely do not change the validity of the results, but a slightly lower overall improvement may be seen in private practice. Although the use of daily text messages only marginally increased patient oral health, the study was constructed in such a way as to provide helpful data to practicing orthodontists. Nearly all orthodontists already stress the importance of daily compliance with hygiene, elastics, and diet – this study supports those statements and leverages current technology to help support patients in those areas. By using multiple messages and by surveying patients regarding message preference, the results of this randomized trial were made more informative. Importantly, the patients themselves received the text message reminders, and the patients reported their preferences, not their parents. In an age when the majority of teenagers have a cell phone, this aspect of the study design is critical. So, for an orthodontist trying to motivate a teenager in braces, what do these data tells us?
Article Reviewed: Mike C. Ross; Phillip M. Campbell; Larry P. Tadlock; Reginald W. Taylor; Peter H. Buschang. Effect of automated messaging on oral hygiene in adolescent orthodontic patients: A randomized controlled trial. Angle Orthodontist. Online 2018. |
Curated by:
Tate H. Jackson, DDS, MS CategoriesArchives
October 2019
|
Copyright © 2016


 RSS Feed
RSS Feed