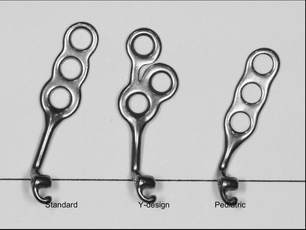
 Bollard Plates with the Y-Design (Center) are recommended. Bollard Plates with the Y-Design (Center) are recommended. BY TUNG T. NGUYEN, DMD, MS The following article outlines our protocol for early treatment of Class III malocclusion using Bone Anchored Maxillary Protraction (BAMP). In a future post, we will include more clinical tips and tricks, as well as information on how to handle unusual complications. Age of the Patient The typical age for BAMP treatment for a patient who has a Class III skeletal relationship with a component of maxillary retorgnathia is 11-14 years. Broadly stated, the younger the patient, the better the chance for orthopedic protraction of the maxilla and midface. The success of BAMP treatment is primarily dependent on 2 factors:
Surgical Management – Placement of the Plates We recommend the Bollard plate with the Y-Design (center plate in the image below). The Standard (screw holes in-line) design can also be used with success. The maxillary bone plates are inserted in the infrazygomatic crest, with the plate arm emerging through attached tissue near the maxillary molars. The mandibular bone plates are inserted between the mandibular lateral incisors and canines – again with the intraoral attachment emerging from attached tissue. For the placement of both the maxillary and mandibular plates, a small flap is raised with a design that maintains good blood flow to the tissue. We refer all plate placement to qualified oral and maxillofacial surgeons familiar with the technique and treatment goals. Ideally 1.5-2.0 mm of cortical plate thickness is needed to ensure both short-term and long-term stability of the plates. For these reasons, we often delay BAMP treatment until the age of 11. In the mandible, extraction of primary canines (M & R) will expedite the eruption of the permanent canine to help provide the inter-radicular space needed for the plates and screws. 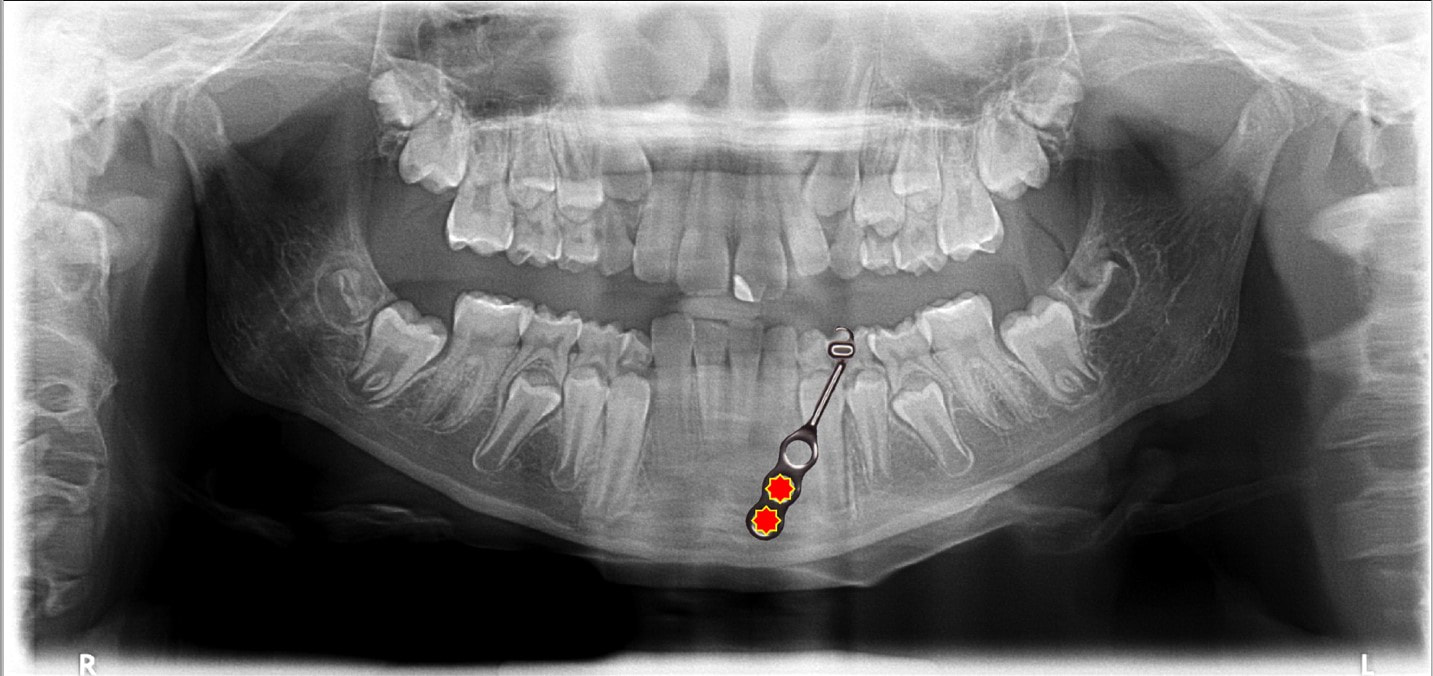 If the permanent mandibular canines have not yet erupted, the mandibular plates can still be placed, however. In these special circumstances, we use the maxillary plates with 3 screw holes (in-line, not the Y-Design) and utilize the bottom 2 screws with the most apical hole placed just beneath the lateral incisor root. The plates are placed with a distal angulation – so that the hooks on the plates still emerge into keratinized gingiva in the region just buccal and apical to where the permanent canine crown will erupt. The screws can either be inserted with the surgeon making small pilot holes or using self-drilling screws. We recommend the use of a pilot hole, as it decreases the mechanical stress on the bone and facilitates faster healing. Orthopedic Traction The plates are loaded 3-4 weeks after surgery, if they are stable. We test stability clinically at each plate before loading. Initial traction is 100g per side for 6 weeks. The patient is instructed to wear the elastics 24/7 and to change the elastics at every meal. Make sure that the patient does not experience sharp or dull nagging pain when wearing the elastics. If the patient experiences sharp pain upon elastic loading, instruct them to discontinue elastic wear immediately. Sharp pain usually indicates plate instability. Stopping traction is most often the best way to allow the plates to re-stabilize. After 6 weeks of initial loading, the traction force can be increased to 150g per side for an additional 6 weeks. The final loading force is 250g per side about 6 weeks later. Often, patients who have a Class III skeletal relationship with a deepbite and anterior crossbite require some sort of bite-opening appliance to allow the crossbite to be most efficiently corrected. To accomplish this goal, we place temporary bite turbos on the mandibular first molars, but a retainer with a posterior bite plate is also effective. Most often, we start BAMP treatment with a full fixed appliance in the lower arch to decompensate the mandibular incisors. Our experience suggests that young patients are more motivated to wear elastics until the anterior crossbite is corrected. By simultaneously decompensating (proclining) the lower incisors with a fixed appliance, we know the true amount of orthopedic correction needed in order to obtain positive overjet with an aligned mandibular arch. Once positive overjet is obtained, we place full maxillary appliances and continue elastics to overcorrect to ~4mm overjet or ½ cusp Class II. Elastics can then be decreased to only night time wear for retention of the orthopedic improvement until mandibular growth is completed. After debond, the patient is seen every 6 months for growth observation. If the overjet decreases, we increase elastic wear to full time in order to help account for continued Class III mandibular growth. In the rare instances in which the overjet increases, the patient can cut elastic wear to every other night. The plates and screws can often be maintained successfully for several years and then removed in conjunction with 3rd molar extractions, if indicated. In summary, the clinical protocol is as follows:
11 Comments
|
Curated by:
Tate H. Jackson, DDS, MS CategoriesArchives
October 2019
|
Copyright © 2016
 RSS Feed
RSS Feed