 CBCT of the same airway with the patient supine (left) and upright (right). Van Holsbeke et al 2014 CBCT of the same airway with the patient supine (left) and upright (right). Van Holsbeke et al 2014 BY TUNG T. NGUYEN Approximately 20% of adults and 2-10% of children suffer from obstructive sleep apnea (OSA). The potential impact to health includes: diabetes, stroke, heart attack, lack of concentration, fatigue, among other symptoms.(1) The financial impact of OSA is estimated at $60 billion dollars annually. These numbers alone might inspire you to embrace the growing trend of “Airway Friendly Orthodontics,” but what do those words really mean? With the potential for truly significant health impacts, it is easy to sensationalize treatment designed to improve the symptoms of OSA in children. What does current evidence suggest? In order to separate fact from fiction, when it comes to OSA in growing patients, the well-informed orthodontist must first understand three basic anatomic and physiological principles regarding airway. 1. Airway volume and cross-sectional area are influenced by head position, consciousness and inhalation/ exhalation state during image capture. The majority of CBCT studies published in orthodontic journals are captured in the upright or sitting position. Yet, airway studies have shown that minimum cross-sectional area decreases by as much as 70% from the upright to supine position.(2) In addition, airway volume and cross-sectional area decrease in unconscious breathing compared to conscious breathing. A single snapshot of the airway captured using CBCT is an anatomic image with limitations: the patient is almost never lying down or asleep. Correctly interpreting data collected in such a fashion means understanding that the true physiologic problem (OSA) might be diminished or amplified relative to the CBCT volume. 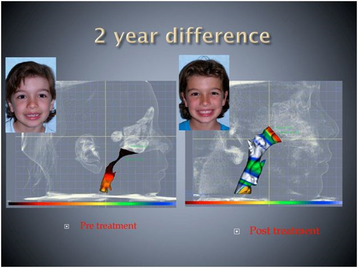 The airway changes with growth. cbctortho.com The airway changes with growth. cbctortho.com 2. Airway volume and minimum cross-sectional area both increase from birth to age 20 years, then stabilize until to the 50s, after which they slowly dcrease.(3) That means that any case report or study in growing patients needs to have untreated controls to separate treatment effect from growth alone. If appliance “X” reportedly increases the airway volume or minimum cross-sectional area in 10-12 year olds, then ideally, that statement should be made based on comparison to a control group. 3. There is often a remission of OSA from middle childhood to late adolescence. A recent longitudinal study reported only 8.7% of children diagnosed with OSA at ages 8-11 y had OSA at 16-19 years(4) They hypothesized that normal growth of the airway self-corrects the problem. This begs the question “Are we taking credit for fixing something that growth takes care of anyway?” In addition, this study found that snoring alone is not a predictor of OSA for middle-childhood patients. What is the take-home message?
References: 1. Lumeng J and Chervin R. Epidemiology of Pediatric Obstructive Sleep Apnea. Proc Am Thorac Soc. 2008; 5: 242–252. 2. Van Holsbeke CS, Verhulst SL, Vos WG, De Backer JW, Vinchurkar SC, Verdonck PR et al. Change in upper airway geometry between upright and supine position during tidal nasal breathing. J Aerosol Med Pulm Drug Deliv. 2014; 27:51–7. 3. Schendel SA, Jacobson R, Khalessi S. Airway growth and development: a computerized 3-dimensional analysis. J Oral Maxillofac Surg. 2012 2012-09-01;70(9):2174–83. 4. Spilsbury, J.C., Storfer-Isser, A., Rosen, C.L. et al, Remission and incidence of obstructive sleep apnea from middle childhood to late adolescence. Sleep. 2015;38:23–29.
3 Comments
|
Think Pieces are longer-form editorials on selected topics.
Curated by:
Tate H. Jackson, DDS, MS Archives
October 2018
Categories |
Copyright © 2016
 RSS Feed
RSS Feed